The Difference Between Bipolar Disorder and Moodiness
People often wonder if they have a diagnosable psychological condition, or if they're just going through a bad spell. How can you tell the difference?
Sometimes people just wake up on the wrong side of the bed. They don’t have enough milk for their cereal, or enough time to finish their coffee before leaving the house, or there’s terrible traffic on the way to work, or there’s some kind of catastrophe on the subway. Sometimes there isn’t even a reason they can point to. They’re just in a crappy mood.
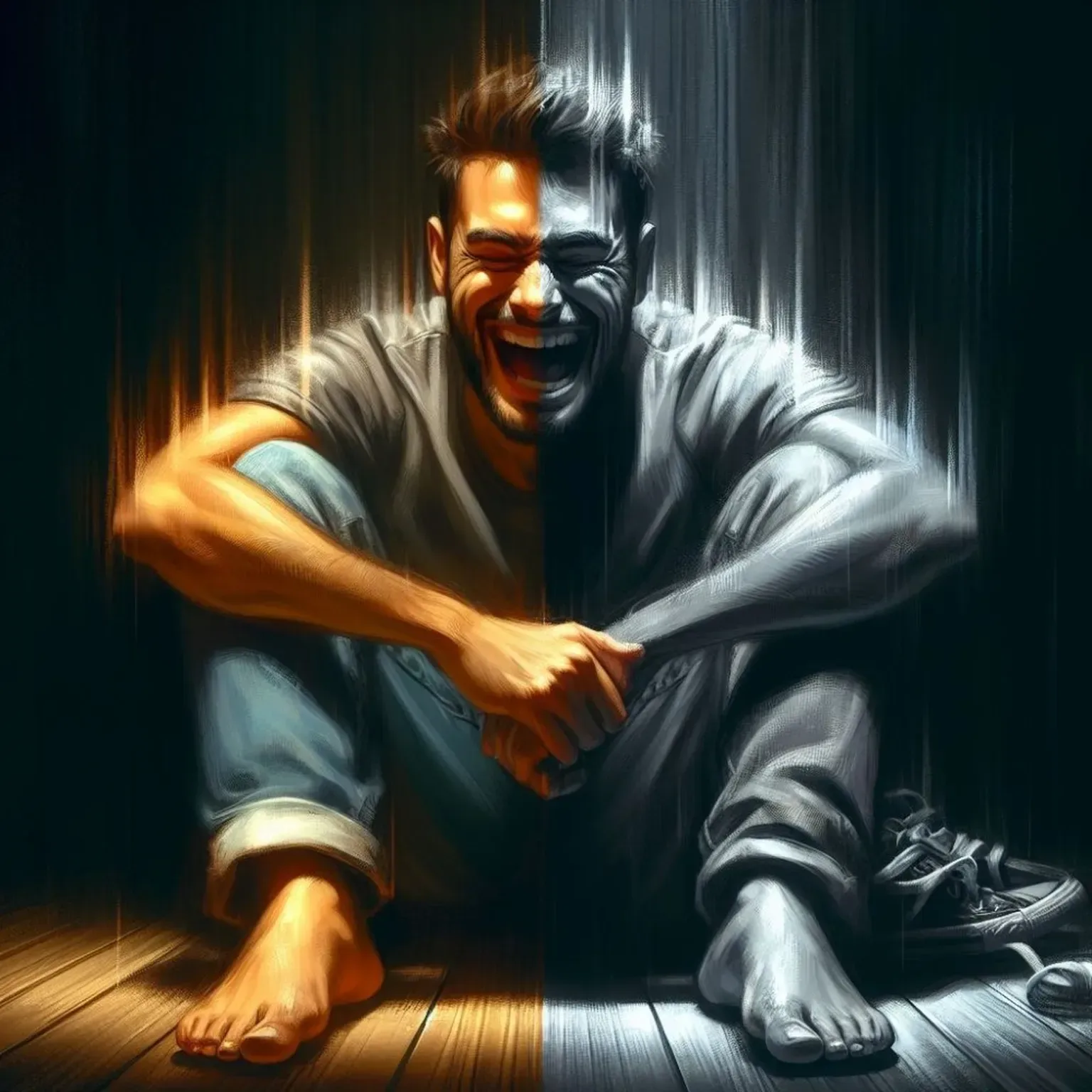
Unless you’re Leslie Knope the above paragraph probably applies to you. Everyone (or almost everyone) has their moods. Of course, there is a big difference between being “in a mood” — or even being “moody” — and having a mood disorder, like being bipolar.
If you’re reading this, chances are that you are wondering whether or not your moods are your average, typical, everyday fluctuations in affect, or if they’re the sign of something more severe. You’re not alone. In fact it’s the question that often brings people to our digital doorstep: am I bipolar, or am I just going through a phase? Hopefully, by the time you’re done reading this article, you’ll have a better sense of where you fit on the psychological spectrum. (And if you don’t, you can always set up an appointment to talk to one of our therapists!)
WHAT IS BIPOLAR DISORDER?
There are two forms of bipolar disorder, bipolar 1 and bipolar 2: both involve an individual’s mood swinging between extremes (or poles).
BIPOLAR 1 DISORDER
Bipolar 1 disorder is diagnosed when individuals experience a period of “mania” that lasts more than a week; during a manic episode people feel extremely energetic and active. They might have racing thoughts that they can’t control. They might lack focus, too, or engage in risky behavior, or become extremely irritable. They might even experience symptoms that are associated with psychosis: disorganized thinking, false beliefs, or hallucinations. A decreased need for sleep is also a hallmark of mania – even with only a few hours of sleep people wake up feeling completely refreshed and raring to go in the morning.
What’s important to note is these changes in behavior are drastic. When you have a manic episode, it almost seems like you’re a different version of yourself — or a different person altogether.
Manic episodes are dangerous for both the individual undergoing it and the loved ones that surround them. Indeed people are often hospitalized while undergoing a manic episode. They become dysfunctional at work, at home with their families, and in social settings; they become so distractible, so energetic, or so irritable, that they’re unable to live up to critical responsibilities.
People with bipolar 1 disorder don’t necessarily undergo depressive episodes. Some will, and many (if not most) will experience periods in which their mood is neutral. On the other hand depressive episodes are a diagnostic criteria for bipolar 2 disorder.
BIPOLAR 2 DISORDER
The diagnostic criteria for bipolar 2 disorder require that the individual has undergone a major depressive episode and what’s called a hypomanic episode — essentially, a less severe version of the kind of manic episode described above. Hypomanic episodes last a minimum of four days, as opposed to a week. Also someone suffering from hypomania might even perform better at their job than normal; they’re more energetic, more “up,” more active than usual. To the outside observer, it might seem like they’re in a better mood than usual. That typically isn’t the case with a manic episode. But beware – much like manic episodes, hypomanic episodes are never innocuous, even if they seem that way.
Major depressive episodes last at least two weeks, and are typified by extreme sadness or despair. An individual undergoing a major depressive episode might feel worthless, or be overwhelmed by a sense of guilt; they might lose interest in things they once loved or isolate themselves from friends and family. Exhaustion or fatigue — plus an increased need for sleep — are also potential symptoms of a major depressive episode, as are restlessness and difficulty concentrating. A change in appetite is another signal. Suicidal ideation (or obsessively thinking about death) is common as well.
Cyclothymic Disorder
Cyclothymic Disorder is kind of like bipolar lite — a milder version, in which an individual’s mood frequently swings from depressive to manic. Importantly though the individual doesn’t meet enough of the criteria to be diagnosed as depressive or hypomanic.
WHAT’S THE DIFFERENCE BETWEEN BEING MOODY AND HAVING BIPOLAR DISORDER?
If, in the process of reading this blog, you’ve started to get freaked out because it feels like we’re writing about you, you shouldn’t worry — not necessarily. The thing about bipolar disorder — the thing about many mental health struggles — is that many people all over the world experience similar symptoms. Which should only make us question why there remains such a stigma around mental health care — a subject for a different post, perhaps.
The question then becomes, how do you know if you have bipolar disorder or not?
The truth is, in order to answer that question, you should absolutely consult with a mental health professional (something that we at Rappore are in a unique position to help you with). Of course, that isn’t going to stop people from diagnosing themselves. So before you go down the rabbit hole, keep these things in mind:
Duration: In order to be diagnosed with bipolar 1, you must experience a state of mania that lasts a week or more; in order to be diagnosed with bipolar 2, you must endure a major depressive episode that lasts at least 2 weeks. Cyclothymic disorder is only diagnosed if an individual experiences consistent mood-swings over the course of 2 years. In other words, you have to undergo prolonged periods of extreme behavior. The kind of simple mood-swing that most of us experience typically do not last this long; nor do they frequently recur, as is the case with bipolar disorder.
Extremity: We talked about one form of extremity above, when we were discussing the idea of duration. But the other thing about bipolar disorder is that changes in mood are so extreme that they affect your ability to function on a social and professional level.
Recurrence: Typically, with bipolar disorders, episodes of mania (or hypomania) and depression begin to form a pattern; if your moods are more sporadic, failing to conform to any kind of temporal framework, chances are you don’t have bipolar disorder
TREATMENT
The good news is there are evidenced-based psychotherapeutic and pharmacological treatments for bipolar disorder. Mood stabilizers are often prescribed to manage manic and depressive episodes. Cognitive Behavioral Therapy (CBT) and interpersonal and social rhythm therapy (IPSRT) are highly effective therapeutic modalities for bipolar disorder.
The therapists at Rappore are equipped to help people who are suffering from bipolar disorder, in addition to many other forms of mental illness. We also have psychopharmacologists on staff who collaborate with our therapists to determine how to treat these disorders pharmacologically. Curious to learn more about Rappore? Click here. Or click here to take our Mental Health Fingerprint questionnaire and get started today.